Acetaminophen (often known by the brand name Tylenol) is one of the most commonly used over-the-counter medicines for pain and fever—even during pregnancy. But like many things, its safety isn’t all black and white. Below is a balanced, evidence-based look at what we know today.
During pregnancy, acetaminophen is often preferred because many stronger pain or fever medicines (like NSAIDs) carry risks for the baby or mother.
🧠 How Acetaminophen Works
Unlike other pain relievers such as ibuprofen or aspirin, which mainly act in the body’s tissues, acetaminophen seems to work mostly in the brain and spinal cord (central nervous system).
Scientists believe acetaminophen helps relieve pain and reduce fever through three main mechanisms:
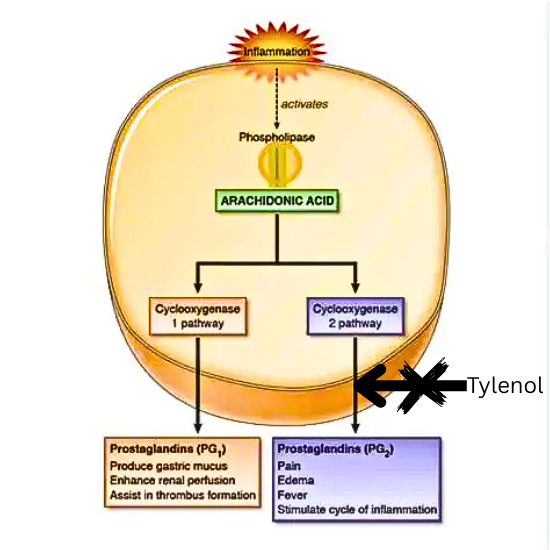
1. 🧬 Blocking Prostaglandin Production (in the Brain)
- Pain and fever are caused partly by prostaglandins, chemicals that tell your brain “Something hurts.”
- Acetaminophen appears to inhibit the enzyme cyclooxygenase (COX)—particularly COX-2—within the brain.
- This reduces prostaglandin production centrally (in the brain) rather than throughout the body, which explains why it doesn’t reduce inflammation like NSAIDs do.
🩺 Result: Less pain and lower fever, but no anti-inflammatory effect.
2. ⚡ Influencing the Serotonin Pathway
- Acetaminophen may increase the activity of serotonin, a neurotransmitter involved in mood and pain control.
- This boost helps the brain dampen pain signals, enhancing its pain-relieving effect.
3. 🌡️ Acting on the Brain’s Thermoregulatory Center
- In the hypothalamus (the brain’s “temperature control center”), acetaminophen helps reset the body’s temperature set-point when you have a fever.
- This signals your body to cool down, usually by sweating and widening blood vessels.
💡 Why It’s Different from Other Pain Relievers
- NSAIDs (like ibuprofen or naproxen) reduce pain, fever, and inflammation.
- Acetaminophen, on the other hand, reduces pain and fever without significant anti-inflammatory effects, which makes it gentler on the stomach and kidneys.
What the Medical Authorities Say
- The FDA (U.S. Food & Drug Administration) and EMA (European Medicines Agency) consider acetaminophen low risk when used properly in pregnancy.
- It remains the first-line option for pain and fever in pregnant women when used as directed.
- ACOG (American College of Obstetricians and Gynecologists) recently reaffirmed: acetaminophen is still the safest choice among available drugs for fever or pain, as long as it’s used at the lowest effective dose and for the shortest time needed.
So, there’s broad consensus in medicine that acetaminophen is “safe enough” when used wisely.
Where the Concerns Come In
In recent years, researchers have raised questions about potential long-term risks when acetaminophen is used frequently or for long periods during pregnancy.
Some observed associations include:
- Neurodevelopmental disorders, such as ADHD and autism. Several meta-analyses have found small increased risks.
- Reproductive / urogenital effects in offspring (though data here are more limited).
- Rare findings, such as prenatal ductus arteriosus closure (a blood vessel in the fetal heart), but these are generally seen in case reports, not large studies.
However, it’s very important to understand:
- These studies are observational (they notice patterns but can’t prove cause and effect).
- Many such studies struggle to fully account for confounding factors—for example, why the drug was used (fever, infection, pain), and other genetic or environmental influences.
- Some more rigorous studies suggest that when you compare siblings (one exposed, one not), the increased risks disappear. For example, a Swedish study found that in sibling-controlled models, there was no increased risk of autism, ADHD, or intellectual disability with acetaminophen use.
What the Largest Studies Show
- In a massive Swedish cohort (nearly 2.5 million children), initial analyses showed small increases in autism and ADHD with acetaminophen exposure. But when siblings were compared, no increased risk was found.
- A meta-analysis pooling many studies showed prenatal acetaminophen exposure was associated with:
• ~30% higher odds of ADHD
• ~19% higher odds of autism spectrum conditions
But again, these numbers reflect associations, not proof that acetaminophen causes these conditions. - A recent review (using the “Navigation Guide” method) concluded that the balance of evidence supports an association between prenatal acetaminophen exposure and increased risk of neurodevelopmental disorders—but emphasized that caution is needed because of study limitations.
- At the same time, leading obstetric groups maintain that current evidence does not justify abandoning acetaminophen when medically needed.
How to Use This Wisely: A Practical Approach
Given both the benefits and the uncertainties, here’s how many clinicians advise pregnant patients:
- Use only when medically necessary — don’t take it “just in case.”
- Lowest effective dose — the smallest amount that helps.
- Shortest duration — take it for as few days as possible.
- Consult your doctor — especially if headaches, fever, or pain are recurring.
- Avoid frequent or prolonged use, unless under close medical supervision.
Bottom Line
- Acetaminophen is still considered the safest over-the-counter pain and fever medicine during pregnancy, under current medical guidelines.
- The best path is a balanced one: use acetaminophen when needed but avoid overuse.
💊 Why Tylenol Is Preferred Over Ibuprofen in Pregnancy
Not all pain relievers are safe during pregnancy.
Ibuprofen and other NSAIDs should be avoided, especially in the second and third trimesters, because they can cause serious problems for the baby — such as:
- 💔 Early closure of a vital blood vessel in the baby’s heart (ductus arteriosus)
- 💧 Low amniotic fluid (oligohydramnios) from reduced kidney function
- ⚠️ Higher risks of miscarriage, growth restriction, or bleeding
These risks become greater after 20 weeks, and especially after 30 weeks of pregnancy.
In contrast, acetaminophen (Tylenol) is considered safer and is the first-choice medicine for pain and fever during pregnancy.
When used as directed — the lowest effective dose for the shortest time needed — it has no proven link to major birth defects or pregnancy complications.
Some recent studies have looked at possible links between frequent Tylenol use and child development issues, but so far, no clear cause-and-effect has been proven.
In summary:
NSAIDs are avoided in pregnancy due to well-known fetal risks.
Tylenol remains the safest and most recommended option when pain or fever needs treatment.
