
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and signs of damage to other organ systems, typically the liver or kidneys. This condition can pose risks to both the mother and baby if left untreated, making awareness and management crucial for expectant mothers.
What is Preeclampsia?
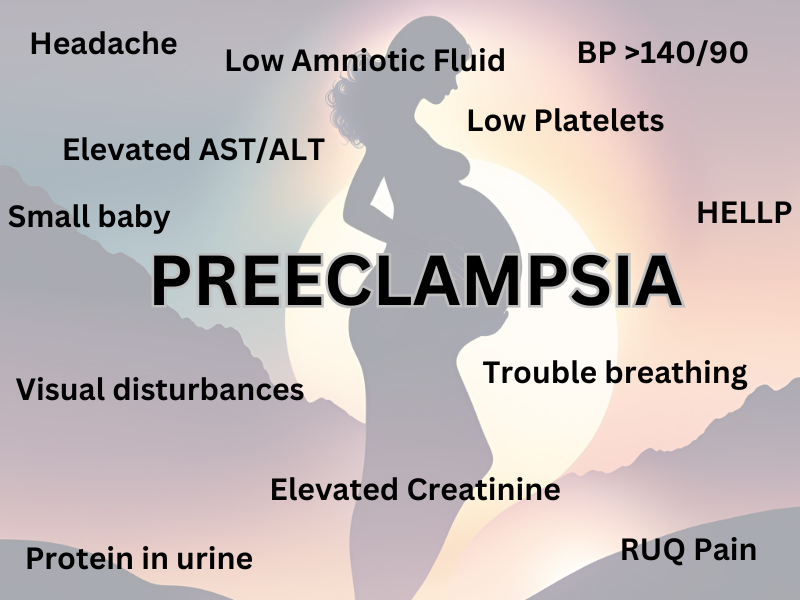
Preeclampsia is a disorder that occurs after 20 weeks of pregnancy, often in the third trimester, though it can sometimes develop earlier or postpartum. It is diagnosed based on:
- Blood pressure readings of ≥140/90 mmHg on two separate occasions at least four hours apart.
- The presence of protein in the urine (≥300 mg in a 24-hour sample) or other signs of organ dysfunction.
In the context of preeclampsia, signs of organ dysfunction extend beyond proteinuria and high blood pressure. These indicators suggest that other organ systems may be affected and often play a role in diagnosis and management. Here are the primary signs of organ dysfunction:
1. Liver Dysfunction
- Elevated liver enzymes: Aspartate transaminase (AST) and alanine transaminase (ALT) levels increase due to liver damage or stress.
- Right upper quadrant or epigastric pain: Often due to liver swelling or stretching of the liver capsule.
2. Kidney Dysfunction
- Proteinuria: Excess protein in the urine (≥300 mg in a 24-hour collection or protein-to-creatinine ratio ≥0.3).
- Elevated serum creatinine: Indicates reduced kidney function, often >1.1 mg/dL or a doubling of baseline levels.
3. Hematologic Dysfunction
- Thrombocytopenia: Low platelet count (<100,000/μL), which can increase the risk of bleeding.
- HELLP Syndrome: A severe form of preeclampsia involving Hemolysis, Elevated Liver enzymes, and Low Platelets.
4. Neurologic Dysfunction
- Severe headaches: Persistent, unrelieved by typical medications, indicating possible cerebral edema or vascular spasm.
- Visual disturbances: Blurred vision, scotomata (blind spots), or sensitivity to light, suggesting potential cerebral or retinal involvement.
- Seizures: Progression to eclampsia, a severe and life-threatening complication of preeclampsia.
5. Respiratory Dysfunction
- Pulmonary edema: Accumulation of fluid in the lungs, leading to shortness of breath or difficulty breathing.
6. Fetal Complications (Reflecting Placental Dysfunction)
- Fetal growth restriction (FGR): Insufficient blood flow to the placenta can impair fetal growth.
- Oligohydramnios: Low amniotic fluid levels due to poor placental function.
7. Cardiovascular Dysfunction
- Elevated blood pressure: Persistent readings ≥160/110 mmHg are considered severe and indicative of significant cardiovascular strain.
8. Gastrointestinal Dysfunction
- Severe nausea or vomiting: Beyond typical pregnancy symptoms, often related to liver or kidney involvement.
These signs help clinicians assess the severity of preeclampsia and determine the need for interventions, including possible early delivery to protect the mother and baby. Regular monitoring and timely management are crucial to prevent progression to severe complications.
When Does Preeclampsia Start?
- Typically: After 20 weeks of pregnancy.
- Early-onset Preeclampsia: Before 34 weeks.
- Postpartum Preeclampsia: Can occur up to 6 weeks after delivery.
Risks of Preeclampsia
For the Mother:
- Organ damage (kidneys, liver, heart).
- Eclampsia (seizures associated with preeclampsia).
- Placental abruption.
- Stroke.
- HELLP syndrome (Hemolysis, Elevated Liver enzymes, Low Platelets).
For the Baby:
- Premature birth.
- Low birth weight.
- Placental insufficiency.
- Stillbirth (in severe cases).
Recognizing Preeclampsia
Symptoms include:
- Severe or persistent headache.
- Blurred vision or sensitivity to light.
- Upper abdominal pain (especially on the right side).
- Swelling in the face, hands, or feet.
- Sudden weight gain.
- Shortness of breath (due to fluid in the lungs).
Risk Factors for Preeclampsia
- Personal history: Previous preeclampsia or hypertension.
- Family history: Preeclampsia in first-degree relatives.
- Medical conditions: Chronic hypertension, diabetes, kidney disease, autoimmune diseases (e.g., lupus).
- Pregnancy factors: First pregnancy, multiple gestation (like twin pregnancy), IVF conception.
- Demographics: Age <18 or >35, obesity, and certain ethnicities.
Management of Preeclampsia
- Monitoring: Frequent blood pressure checks, ultrasounds, and lab tests (liver function, kidney function, platelets).
- Medications:
- Antihypertensives: To control blood pressure (e.g., labetalol, nifedipine).
- Magnesium sulfate: To prevent seizures in severe cases, to treat seizures in other cases.
- Delivery: The only definitive cure for preeclampsia is delivery of the baby. Timing depends on gestational age and severity.
- Mild Preeclampsia: Delivery at or after 37 weeks.
- Severe Preeclampsia: May require early delivery, sometimes before 34 weeks.
Reducing Risk and Preventing Recurrence
- Low-Dose Aspirin (ASA): Recommended for high-risk patients (81 mg daily starting between 12-16 weeks), continued until delivery.
- Healthy Lifestyle:
- Maintaining a healthy weight.
- Watching weight gain.
- Regular exercise.
- Managing chronic conditions (e.g., hypertension, diabetes).
- Calcium Supplementation: In populations with low dietary calcium intake.
Postpartum Risks
- Postpartum Hypertension: Can persist or develop after delivery.
- Long-Term Risks: Women with preeclampsia have an increased risk of chronic hypertension, heart disease, and stroke later in life.
Risk of Recurrence
- Recurrence risk depends on the severity and timing of preeclampsia in the previous pregnancy.
- Mild, late-onset: Lower recurrence risk.
- Severe, early-onset: Higher recurrence risk.
Labs for Diagnosis and Monitoring
- Urine tests: To detect proteinuria.
- Blood tests: Liver function (AST, ALT), kidney function (creatinine), and platelet count.
- Fetal assessments: Ultrasound, Doppler studies for placental blood flow.
Medications: Risks and Benefits

- Labetalol:
- Benefits: Effective in lowering blood pressure quickly.
- Risks: Can cause fatigue, dizziness.
- Nifedipine:
- Benefits: Oral option for blood pressure management.
- Risks: May cause flushing or headache.
- Magnesium Sulfate:
- Benefits: Prevents seizures.
- Risks: Can cause nausea, flushing, or rare toxicity.
- Aspirin:
- Benefits: Reduces the risk of preeclampsia in high-risk patients.
- Risks: Minimal when used at low doses.
The Risk for Preeclampsia following Delivery (Postpartum period):
The risk for preeclampsia persists after delivery due to the lingering effects of the physiological and hormonal changes associated with pregnancy. While delivery of the baby and placenta is the definitive treatment for preeclampsia, the condition can persist or even develop postpartum (known as postpartum preeclampsia). Here’s why:
1. Persistent Vascular Dysfunction
- During pregnancy, preeclampsia involves widespread endothelial dysfunction, where the blood vessel lining becomes inflamed and compromised.
- This dysfunction may not resolve immediately after delivery, leading to continued high blood pressure and risk of complications such as stroke, pulmonary edema, or seizures (eclampsia).
2. Hormonal Changes
- The rapid hormonal shifts that occur after delivery, including drops in progesterone and other pregnancy-related hormones, can exacerbate vascular instability and blood pressure regulation issues.
3. Retained Placental Factors
- Preeclampsia is closely linked to the placenta, which releases proteins that trigger inflammation and vascular problems. After delivery, these proteins may remain in the maternal circulation for a short time, continuing to affect the mother’s body.
4. Fluid Shifts
- After delivery, significant fluid shifts occur in the body as pregnancy-related blood volume decreases. These changes can overload the cardiovascular system, leading to hypertension or pulmonary edema in women predisposed to preeclampsia.
5. Delayed Organ Recovery
- Organs such as the liver and kidneys, which may have been affected during preeclampsia, require time to recover fully. This delay can prolong symptoms and increase risks postpartum.
6. Increased Risk for Postpartum Hypertension
- Some women with preeclampsia develop postpartum hypertension, which can persist for weeks after delivery. This may require ongoing treatment and monitoring.
Postpartum Risks Associated with Preeclampsia
- Eclampsia (Seizures): Postpartum eclampsia can occur even in women without severe preeclampsia during pregnancy.
- Stroke: Elevated blood pressure increases the risk of hemorrhagic or ischemic stroke.
- Pulmonary Edema: Fluid overload can lead to respiratory distress.
- Heart Failure: Rarely, women can develop cardiomyopathy due to the strain on the heart during and after pregnancy.
How Long Does the Risk Last?
- Postpartum preeclampsia can develop up to 6 weeks after delivery, with most cases occurring within the first 48–72 hours. However, complications related to preeclampsia can arise later, emphasizing the need for continued monitoring.
What Can Help Reduce Postpartum Risk?
- Blood Pressure Monitoring: Close observation of blood pressure in the hospital and at home postpartum.
- Medications: Antihypertensives like labetalol or nifedipine to control blood pressure, and magnesium sulfate to prevent seizures if needed.
- Prompt Medical Attention: Recognizing warning signs such as severe headache, vision changes, or difficulty breathing.
- Follow-Up Care: Regular postpartum check-ups to manage lingering hypertension and assess recovery.
Long-Term Risks
Preeclampsia is not just a temporary condition; it also increases the risk of long-term health issues, including:
- Chronic hypertension.
- Cardiovascular disease (e.g., heart attack, stroke).
- Kidney disease.
Women with a history of preeclampsia should maintain regular health check-ups to monitor these risks and adopt lifestyle changes (diet, exercise, stress management) to reduce future complications.
Conclusion
Preeclampsia is a complex condition requiring close monitoring and management to ensure the safety of both mother and baby. Early recognition, risk factor management, and timely delivery are key. Recognizing that the risk persists postpartum is essential. Discussing your risk factors and preventive measures with your healthcare provider can significantly improve outcomes for current and future pregnancies.

One Response