Menopause is a natural biological process that marks the end of a woman’s reproductive years. While it’s a universal experience for all women, the way it manifests and its impact can vary widely. This guide will walk you through what menopause is, its stages, symptoms, causes, and management strategies to help you navigate this life transition confidently.
Menopause is a natural and normal stage of life, marking the transition from a woman’s reproductive years to a new phase of growth and wisdom. It is not an illness but a biological milestone that every woman experiences. While some symptoms may require management, they do not define menopause itself. Embracing this phase with understanding and care allows women to focus on maintaining health, celebrating their journey, and thriving in this new chapter.
The word menopause has its roots in Greek. It is derived from two Greek words:
- “Menos” (μήν) meaning “month,” which relates to the monthly menstrual cycle.
- “Pausis” (παύσις) meaning “cessation” or “stopping.”
Combined, menopause literally means the “cessation of monthly cycles,” which accurately describes the end of a woman’s menstrual periods and reproductive capability.
What is Menopause?
Menopause is defined as the permanent cessation of menstrual periods, occurring when the ovaries stop releasing eggs and producing key hormones like estrogen and progesterone. It is confirmed after 12 consecutive months without a menstrual period. However, menopause does not happen suddenly—it is a gradual process. During the perimenopause phase, which precedes menopause, women may experience irregular or skipped periods as hormone levels fluctuate. Symptoms such as hot flashes, mood changes, and sleep disturbances can also begin during this transitional phase, often well before menopause itself.
Age of Onset:
- Typical Age: Between 45 and 55 years (average age of menopause in the US is age 52).
- Early Menopause: Before age 40.
- Late-Onset Menopause: After age 55.
Stages of Menopause
- Perimenopause (Transition Stage):
- Begins several years before menopause when hormone levels start fluctuating.
- Symptoms like irregular periods, hot flashes, mood swings, trouble sleeping often begin here.
- Menopause:
- Officially starts 12 months after the last menstrual period.
- Postmenopause:
- The period after menopause, where symptoms may persist due to low, and often still somewhat fluctuating hormone levels.
Symptoms of Menopause
Menopause affects women physically, emotionally, and mentally. Common symptoms include:
1. Vasomotor Symptoms:
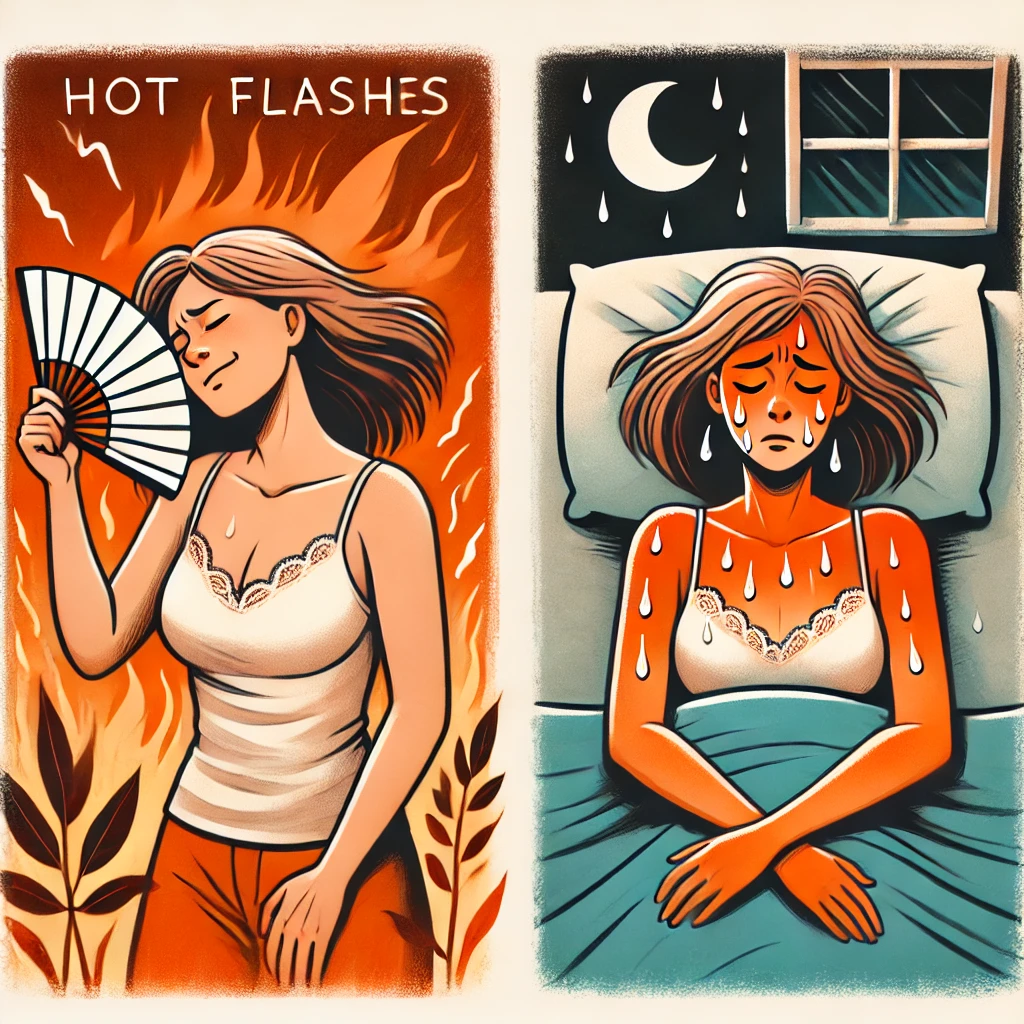
These are among the most common and noticeable symptoms of menopause and perimenopause. These symptoms are caused by changes in the body’s temperature regulation due to fluctuating and declining estrogen levels, which affect the hypothalamus, the part of the brain that controls body temperature. Here’s a breakdown of these symptoms:
1. Hot Flashes
- What They Are: Sudden feelings of intense warmth, often starting in the chest or face and spreading to the rest of the body.
- Duration: Typically last 1–5 minutes.
- When They Occur: Can happen during the day or night (referred to as night sweats when they disturb sleep).
- Triggers: Can be exacerbated by stress, spicy foods, alcohol, caffeine, or warm environments.
2. Night Sweats
- What They Are: Episodes of excessive sweating during sleep, often drenching clothing or bed linens.
- Impact: Can disrupt sleep, leading to fatigue, irritability, and difficulty concentrating during the day.
3. Flushing
- What It Is: A sudden redness of the skin, often on the face, neck, or chest, sometimes accompanied by perspiration.
- Related to Hot Flashes: Often occurs simultaneously with or as part of a hot flash.
4. Chills
- What They Are: Feeling cold or shivering, which can follow a hot flash as the body adjusts its temperature.
Frequency and Duration
- Common in Menopause: Affect up to 75% of women during menopause.
- Duration of Symptoms: While most women experience vasomotor symptoms for 6 months to 2 years, some may have symptoms for a decade or longer.
Management of Vasomotor Symptoms
Lifestyle Modifications
- Keep cool: Use fans, wear lightweight clothing, and avoid hot environments.
- Avoid triggers: Limit caffeine, alcohol, and spicy foods.
- Manage stress: Practice relaxation techniques like yoga, meditation, or deep breathing.
Medical Treatments
- Hormone Therapy (HT): Estrogen therapy (alone or with progesterone) is highly effective for managing hot flashes and night sweats.
- Non-Hormonal Options:
- SSRIs or SNRIs (e.g., venlafaxine, paroxetine) can reduce hot flashes.
- Gabapentin or clonidine for severe cases.
Alternative Therapies
- Acupuncture: May provide relief for some women.
- Herbal remedies: Black cohosh or phytoestrogens (consult a doctor before use).
Vasomotor symptoms can significantly impact quality of life, but they are manageable with the right approach. If symptoms are severe or interfere with daily life, consulting a healthcare provider can help identify the best treatment options.
2. Menstrual Changes:

- One of the earliest and most noticeable signs of approaching menopause is a change in menstrual cycles. These changes occur during perimenopause, the transitional phase leading up to menopause, as the ovaries begin to produce less estrogen and progesterone. Hormonal fluctuations during this time can cause periods to become irregular in several ways:
1. Irregular Timing
Cycles may become shorter (less than 21 days) or longer (more than 35 days).
You might skip periods entirely for a month or more, followed by a return to normal or heavier-than-usual cycles.
2. Changes in Flow
Heavier periods: Known as menorrhagia, this can occur due to prolonged exposure to estrogen without the balancing effect of progesterone.
Lighter periods: Hormonal levels may not be sufficient to build a thick uterine lining, resulting in reduced bleeding.
3. Spotting Between Periods
Some women may experience spotting or light bleeding between cycles due to hormonal imbalances or structural issues like polyps or fibroids.
4. Prolonged or Shortened Period Duration
Periods may last longer than 7 days or may be brief, lasting just 1–2 days.
Why These Changes Happen
Hormonal fluctuations during perimenopause disrupt the regular patterns of ovulation, leading to inconsistent production of estrogen and progesterone.
Without consistent ovulation, the uterine lining may thicken excessively or shed incompletely, resulting in variable bleeding patterns.
When to Seek Medical Attention
While menstrual changes are a normal part of perimenopause, consult a healthcare provider if you experience:
Extremely heavy bleeding (soaking through a pad or tampon every hour).
Bleeding that lasts more than 7–10 days.
Bleeding after menopause (12 months of no periods).
Severe pain or significant clots.
Management and Relief
Lifestyle Changes: Maintain a healthy diet and exercise regularly to support hormonal balance.
Medical Options: Hormonal treatments like birth control pills, IUDs, or progesterone therapy to regulate cycles.
Non-hormonal treatments like NSAIDs or Tranexamic Acid to reduce heavy bleeding.
Menstrual changes are a natural part of the transition to menopause. Monitoring your cycles and symptoms can help you and your healthcare provider determine whether they are within the normal range or if further evaluation is needed. These symptoms can always be managed if you so choose.
3. Vaginal and Urinary Symptoms in Menopause
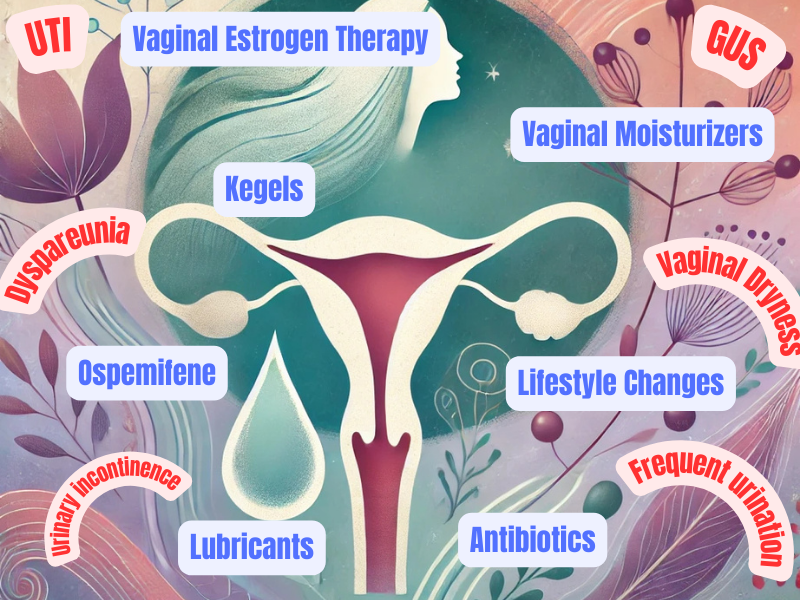
As women transition through menopause, declining estrogen levels can cause significant changes in the vaginal and urinary tissues. These changes are part of a condition known as genitourinary syndrome of menopause (GSM), which encompasses a range of symptoms affecting the vagina, vulva, and urinary system. Here’s an expanded look at these symptoms:
Vaginal Dryness
- Cause: The drop in estrogen levels leads to thinning and loss of elasticity in the vaginal walls. It also reduces the production of natural lubrication.
- Symptoms: Dryness, irritation, itching, or a feeling of tightness in the vaginal area.
- Impact: Can lead to discomfort during daily activities and significantly affect sexual health.
Pain During Intercourse (Dyspareunia)
- Cause: Thinning vaginal tissues (vaginal atrophy) and reduced lubrication result in less elasticity and increased sensitivity during intercourse.
- Symptoms: Burning, stinging, or tearing sensations during or after sexual activity.
- Impact: May lead to decreased sexual satisfaction, avoidance of intimacy, and emotional strain in relationships.
Increased Risk of Urinary Tract Infections (UTIs)
- Cause: Lower estrogen levels thin the urinary tract lining and disrupt the vaginal flora (including a reduction in protective lactobacilli), allowing harmful bacteria to thrive.
- Symptoms: Frequent urination, burning sensation, and urgency.
- Impact: Recurring UTIs can cause discomfort and require frequent medical treatment.
Other Related Symptoms
- Urinary Incontinence: Weakening of the pelvic floor muscles and changes in the bladder lining may result in leakage during coughing, sneezing, or physical activity (stress incontinence).
- Frequent Urination: Hormonal changes can irritate the bladder, leading to an increased need to urinate.
Management and Treatment Options
1. Vaginal Estrogen Therapy
- What It Does: Delivers low-dose estrogen directly to the vaginal tissues to restore moisture, elasticity, and pH balance.
- Forms Available: Creams, tablets, or a vaginal ring.
2. Over-the-Counter Products
- Vaginal Moisturizers: For long-lasting hydration and daily comfort.
- Lubricants: To reduce friction and discomfort during intercourse (water- or silicone-based options are best).
3. Pelvic Floor Exercises (Kegels)
- Strengthens pelvic muscles to reduce incontinence and improve bladder control.
4. Lifestyle Changes
- Stay hydrated to maintain urinary tract health.
- Avoid irritants like caffeine, alcohol, and spicy foods that may worsen bladder symptoms.
5. Probiotics
- Support vaginal and urinary health by maintaining a healthy balance of protective bacteria.
6. Prescription Medications
- Ospemifene: A selective estrogen receptor modulator (SERM) used to treat painful intercourse due to vaginal atrophy.
- Antibiotics: For treating recurrent UTIs.
7. Non-Hormonal Therapies
- Laser treatments like vaginal rejuvenation (e.g., MonaLisa Touch) to restore vaginal tissue health.
When to Seek Medical Help
Consult your healthcare provider if:
- Vaginal or urinary symptoms significantly affect your quality of life.
- You experience frequent UTIs or unusual urinary symptoms.
- Over-the-counter treatments do not provide sufficient relief.
With the right management, vaginal and urinary symptoms of menopause can be alleviated, ensuring comfort, improved sexual health, and better overall quality of life.
4. Emotional and Cognitive Changes During Menopause
Menopause is not just a physical transition—it also brings significant emotional and cognitive changes for many women. These changes are influenced by fluctuating hormone levels, particularly a decline in estrogen, which affects neurotransmitters in the brain. Understanding these symptoms can help women navigate this life stage with greater awareness and support.
Emotional Changes
The hormonal shifts of menopause can have a profound impact on mood and emotional well-being.
Mood Swings
- What Happens: Sudden and intense changes in mood, ranging from happiness to sadness or irritability, often without a clear cause.
- Why It Occurs: Fluctuations in estrogen affect serotonin and dopamine, neurotransmitters that regulate mood.
- Impact: Can lead to feelings of frustration or unpredictability, sometimes causing strain in personal relationships.
Irritability or Anxiety
- What Happens: Increased sensitivity, feelings of restlessness, or worry that may feel overwhelming.
- Why It Occurs: Declining hormone levels disrupt the stress response, making women more susceptible to anxiety.
- Impact: Anxiety may manifest as a constant sense of unease, difficulty relaxing, or even physical symptoms like a racing heart.
Cognitive Changes
Menopause can also affect mental clarity and cognitive function, often referred to as “menopause brain” or “brain fog.”
Memory Lapses
- What Happens: Forgetting names, misplacing items, or struggling to recall words or details.
- Why It Occurs: Estrogen plays a key role in brain function, including memory. Declining levels may temporarily affect cognitive performance.
- Impact: While typically mild, memory lapses can lead to frustration or self-doubt.
Difficulty Concentrating
- What Happens: Trouble focusing on tasks, following conversations, or completing complex projects.
- Why It Occurs: Hormonal changes combined with sleep disturbances, anxiety, and stress can make it harder to concentrate.
- Impact: Can affect productivity at work or home, contributing to feelings of being overwhelmed.
Underlying Factors That Worsen Symptoms
- Sleep Disturbances: Night sweats and insomnia reduce sleep quality, amplifying emotional and cognitive challenges.
- Stress: Life transitions during menopause, such as aging parents, children leaving home, or work pressures, can heighten emotional strain.
- Thyroid Dysfunction: Often mistaken for menopause symptoms, thyroid issues can exacerbate mood swings and brain fog.
Managing Emotional and Cognitive Symptoms
Lifestyle Changes
- Regular Exercise: Improves mood, reduces stress, and boosts cognitive function. Aerobic activities like walking or swimming are particularly helpful. Yoga is simply amazing.
- Healthy Diet: A balanced diet rich in omega-3 fatty acids, antioxidants, and whole grains supports brain health and mood stability.
- Sleep Hygiene: Maintain a consistent sleep schedule, create a calming bedtime routine, and limit caffeine or alcohol in the evening.
Stress Management
- Mindfulness and Meditation: Help reduce anxiety and improve focus.
- Yoga or Tai Chi: Combines physical movement with relaxation techniques.
There are many online options for this. Here is one: https://youtu.be/0PJPNiveIU8?si=-ZTK8aW2uhia2i3p
Therapeutic Interventions
- Hormone Therapy (HT): Estrogen replacement can help regulate mood and cognitive symptoms for some women.
- Antidepressants or Anti-Anxiety Medications: Selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) can help manage severe mood swings or anxiety.
- Cognitive Behavioral Therapy (CBT): Proven to reduce menopausal anxiety, depression, and stress.
Supplements and Natural Remedies
- Vitamin B Complex: Supports brain health and energy levels.
- Omega-3 Fatty Acids: Found in fish oil, can improve cognitive function and reduce mood swings.
- Herbal Remedies: Black cohosh or valerian root may provide relief, though evidence is mixed; consult your doctor before use.
Social and Emotional Support
- Support Groups: Talking to other women experiencing menopause can normalize symptoms and provide emotional relief.
- Open Communication: Sharing your feelings with family or friends can foster understanding and reduce isolation.
When to Seek Medical Advice
While emotional and cognitive changes are common, consult a healthcare provider if:
- Mood swings or anxiety interfere with daily life.
- Memory problems or concentration difficulties worsen or persist beyond menopause.
- To be sure there no other underlying conditions, such as depression or thyroid issues.
Conclusion
Emotional and cognitive changes during menopause are a normal part of this life transition but can feel overwhelming without proper support. Through lifestyle adjustments, medical treatments, and emotional support, women can manage these challenges effectively and maintain their overall well-being.
5. Physical Changes During Menopause
Menopause brings many changes to the body as hormone levels shift, especially the decline in estrogen and progesterone. These hormonal changes affect the body in various ways, often resulting in noticeable physical differences. Here’s a breakdown of the most common physical changes:
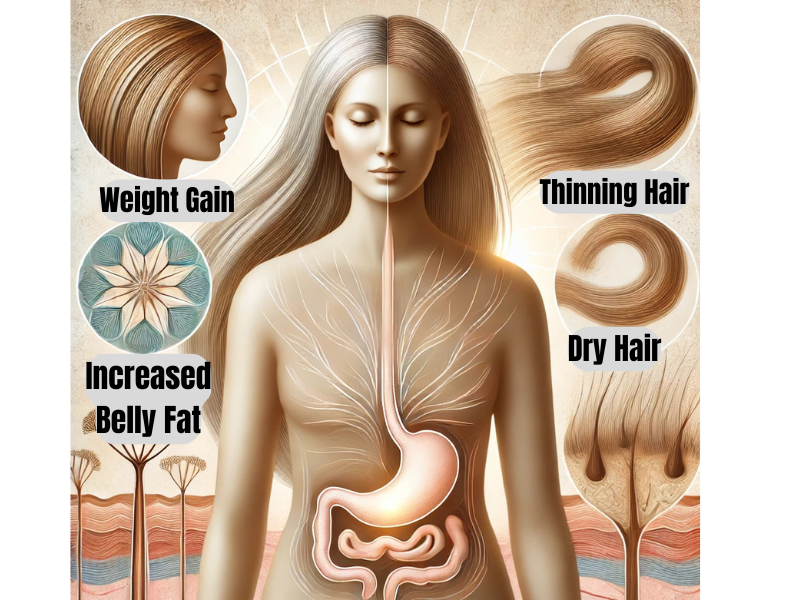
Weight Gain, Especially Around the Abdomen
- What Happens: Many women notice that they gain weight more easily during menopause, particularly in the abdominal area. This is often referred to as “belly fat.”
- Why It Happens:
- The decline in estrogen alters how the body stores fat, shifting it from the hips and thighs to the abdomen.
- Metabolism naturally slows with age, making it harder to burn calories.
- Loss of muscle mass (due to aging and reduced physical activity) contributes to slower calorie-burning.
- What You Can Do:
- Healthy Diet: Focus on whole grains, lean proteins, fruits, and vegetables while limiting processed foods and added sugars.
- Regular Exercise: Incorporate strength training and cardio to maintain muscle mass and support weight management.
- Manage Stress: High stress levels can increase cortisol, a hormone that promotes fat storage.
Thinning Hair or Hair Loss
- What Happens: Hair may become thinner overall, and some women experience noticeable hair loss, especially at the crown or temples.
- Why It Happens:
- Lower estrogen levels disrupt the natural hair growth cycle, shortening the growth phase (anagen) and leading to more shedding.
- An increase in androgens (male hormones) can cause hair follicles to shrink, resulting in thinner hair.
- What You Can Do:
- Healthy Hair Care: Use gentle shampoos and conditioners, avoid harsh styling products, and limit heat treatments like blow-drying or straightening.
- Dietary Support: Ensure adequate intake of protein, biotin, zinc, and omega-3 fatty acids to promote healthy hair growth.
- Medical Options: Minoxidil (Rogaine) is an FDA-approved treatment for hair thinning in women. Consult a doctor for personalized advice.
Dry Skin and Decreased Elasticity
- What Happens: Skin may feel dry, rough, or itchy, and it may lose its firmness and elasticity, leading to fine lines and wrinkles.
- Why It Happens:
- Estrogen helps maintain skin hydration and collagen production. When estrogen levels decline, the skin loses moisture and collagen, resulting in dryness and less elasticity.
- Slower cell turnover and reduced oil production contribute to these changes.
- What You Can Do:
- Hydration: Drink plenty of water and use moisturizers containing hyaluronic acid or ceramides to lock in hydration.
- Sun Protection: Always use sunscreen to prevent further skin damage and maintain elasticity.
- Healthy Fats: Include foods rich in healthy fats, like avocados, nuts, and seeds, to support skin health.
- Exfoliation: Gently exfoliate to remove dead skin cells and promote cell renewal, but avoid over-exfoliating, which can irritate dry skin.
Tips for Managing Physical Changes
These physical changes are a natural part of menopause, but with a proactive approach, you can manage them effectively and maintain your confidence and well-being.
6. Sleep Disturbances During Menopause
Sleep disturbances are a common challenge for women during menopause and perimenopause, often disrupting rest and overall quality of life. Hormonal fluctuations, particularly the decline in estrogen and progesterone, play a significant role in these issues. Here’s an expanded look at what causes these disturbances and how to manage them effectively.
What are Sleep Disturbances?
- Difficulty Falling Asleep: Taking longer than usual to transition into sleep.
- Difficulty Staying Asleep: Frequent waking during the night, often accompanied by trouble falling back asleep.
- Early Morning Waking: Waking up too early and being unable to return to sleep.
- Poor Sleep Quality: Feeling unrested despite spending enough time in bed.
Why Do Sleep Disturbances Happen?
Sleep problems during menopause often stem from a combination of hormonal, physical, and psychological factors:
1. Hormonal Changes
- Decline in Estrogen: Estrogen helps regulate the sleep cycle by influencing serotonin production and body temperature. Its reduction can lead to poor sleep quality.
- Progesterone Fluctuations: Known for its calming effect, the drop in progesterone may contribute to difficulty relaxing and falling asleep.
2. Night Sweats and Hot Flashes
- Sudden waves of heat and sweating at night can wake women up, disrupting their sleep cycles.
3. Anxiety and Stress
- Increased feelings of anxiety and mood changes during menopause can make it harder to unwind and fall asleep.
4. Physical Discomfort
- Joint pain, muscle aches, or urinary symptoms like frequent urination may interrupt sleep.
5. Age-Related Changes
- As women age, natural changes in the circadian rhythm and lighter sleep patterns can exacerbate sleep issues.
Impact of Sleep Disturbances
- Daytime Fatigue: Feeling tired and drained, which affects productivity and energy levels.
- Mood Swings: Poor sleep can worsen irritability, anxiety, and depression.
- Cognitive Impairment: Lack of restful sleep may lead to memory problems or difficulty concentrating.
- Health Risks: Chronic sleep deprivation is associated with an increased risk of heart disease, high blood pressure, and weakened immunity.
How to Manage Sleep Disturbances
1. Lifestyle Changes
- Maintain a Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends.
- Create a Relaxing Bedtime Routine: Include calming activities like reading, meditation, or a warm bath.
- Optimize Your Sleep Environment: Keep the bedroom cool, dark, and quiet, and invest in comfortable bedding.
2. Diet and Exercise
- Limit Caffeine and Alcohol: Avoid these substances, especially in the evening, as they can disrupt sleep.
- Eat Light at Night: Heavy meals close to bedtime can cause discomfort and impact sleep.
- Exercise Regularly: Regular physical activity, especially earlier in the day, promotes better sleep quality.
3. Hormone Therapy (HT)
- Estrogen therapy may reduce hot flashes and night sweats, leading to better sleep. Discuss risks and benefits with your doctor.
4. Non-Hormonal Medications
- Melatonin: Helps regulate sleep-wake cycles and improve sleep onset.
- Prescription Sleep Aids: For severe cases, short-term use of medications like Zolpidem may be an option. Risks and benefits always have to be weighed against each other.
5. Cognitive Behavioral Therapy for Insomnia (CBT-I)
- A structured, evidence-based approach to address the thoughts and behaviors that interfere with sleep.
6. Natural Remedies
- Herbal Supplements: Valerian root, chamomile, or lavender may promote relaxation. Consult a healthcare provider before use.
- Mindfulness Practices: Yoga, tai chi, and deep breathing exercises can reduce stress and improve sleep.
When to Seek Help
If sleep disturbances significantly affect your daily life or persist despite lifestyle changes, consult a healthcare provider. They can help identify underlying issues and recommend appropriate treatments.
Conclusion
Sleep disturbances during menopause are a common but manageable issue. By addressing hormonal changes, adopting healthy habits, and exploring treatment options, women can improve their sleep quality and overall well-being during this transitional phase.
Causes of Menopause
Menopause is primarily caused by a decline in the reproductive hormones estrogen and progesterone.
Other Causes Include:
- Surgical Menopause: Removal of ovaries (oophorectomy).
- Medical Treatments: Chemotherapy or radiation therapy.
- Primary Ovarian Insufficiency (POI): When ovaries stop functioning before age 40.
Other Health Risks Associated with Menopause
The drop in estrogen levels during menopause can lead to long-term health risks, including:
- Osteoporosis:
- Reduced bone density increases the risk of fractures.
- Cardiovascular Disease:
- Higher risk of heart disease due to lower estrogen levels.
Diagnosing Menopause
- Symptom Assessment: Based on irregular periods, cessation of menstrual cycles for 12 months or more and classic symptoms like hot flashes.
- Blood Tests (If Needed):
- Follicle-stimulating hormone (FSH) levels.
- Estrogen levels.
- Thyroid function tests or other tests (to rule out other causes).
Managing Menopause Symptoms
Menopause can’t be stopped, but symptoms can be managed effectively through lifestyle changes, medications, and therapies.
Lifestyle Changes
- Diet:
- Eat calcium and vitamin D-rich foods to strengthen bones.
- Include whole grains, fruits, and vegetables for overall health.
- Exercise:
- Weight-bearing exercises for bone health.
- Yoga or meditation for stress and mood management.
- Hydration:
- Stay hydrated to combat dryness and flush toxins.
- Quit Smoking and Limit Alcohol:
- Reduces hot flashes and lowers health risks.
Hormone Therapy (HT):
- Estrogen Therapy:
- Effective for managing hot flashes and vaginal symptoms.
- May carry risks like blood clots or breast cancer; discuss with your doctor.
- Combination Therapy:
- Estrogen and progesterone for women with an intact uterus to prevent uterine cancer.
Non-Hormonal Medications:
- Antidepressants: SSRIs or SNRIs for hot flashes and mood swings.
- Gabapentin: For hot flashes.
- Vaginal Estrogen Creams: To relieve dryness and discomfort.
Supplements:
- Calcium and Vitamin D: For bone health.
- Omega-3 Fatty Acids: For heart health and mood.
Alternative Therapies:
- Herbal Remedies: Black cohosh or red clover for hot flashes (consult your doctor first).
- Acupuncture: May help with sleep and mood regulation.
When to See a Doctor
Consult a healthcare provider if you experience:
- Severe or persistent symptoms affecting your quality of life.
- Abnormal vaginal bleeding after menopause.
- Signs of osteoporosis (fractures, back pain).
Postmenopausal Health
After menopause, women should focus on preventive care to maintain health:
- Bone Health:
- Regular bone density scans (DEXA).
- Cardiovascular Health:
- Monitor cholesterol and blood pressure.
- Cancer Screening:
- Regular mammograms and Pap smears.
- Mental Health:
- Address symptoms of anxiety or depression.
Conclusion
Menopause is a natural transition, but it can bring physical and emotional challenges. Understanding what to expect and adopting healthy habits can help you navigate this phase with confidence. If symptoms are severe or disruptive, a healthcare provider can offer treatments tailored to your needs, ensuring a smoother transition to postmenopausal health.
For more guidance, tips, and support, consider consulting your OB/GYN to create a plan that works best for you.
