Ladies, let’s talk about ovarian cysts. You’ve probably heard the term before, but what are they? Are they scary? Do you need to freak out if you’ve got one? Let’s break it all down in a way that makes sense.
What Are Ovarian Cysts?
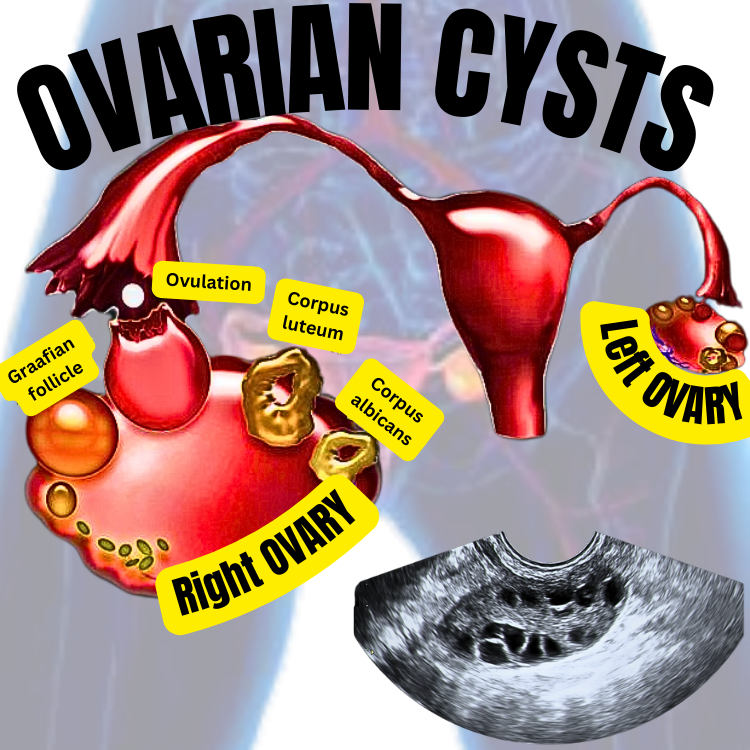
Imagine your ovaries as little egg factories (which, in fact, they are). Sometimes, these factories can get creative and make something extra: a cyst. A cyst is a fluid-filled sac that pops up on or inside an ovary.
Most of the time, these cysts are no big deal—they’re just freeloaders hanging out. But every now and then, they can cause a bit of drama.
Types of Ovarian Cysts
Not all cysts are created equal. Here are the main types:
A)Functional Cysts (a.k.a. “Normal Cysts”): The Common Culprits
Functional cysts are the most common type of ovarian cysts and are typically part of the normal menstrual cycle. They form because of how your ovaries work to prepare and release eggs each month. There are two main types:
- Follicular Cyst:
- Normally, every menstrual cycle, your ovary grows a tiny fluid-filled sac called a follicle. This follicle acts like an egg incubator, helping the egg mature before it’s released during ovulation.
- Sometimes, the follicle gets stage fright—it doesn’t release the egg as it should. Instead, it keeps growing, turning into a follicular cyst.
- Most of the time, these cysts are small, painless, and don’t cause any symptoms. They typically disappear within a month or two without you even realizing they were there.
- Corpus Luteum Cyst:
- A corpus luteum cyst is a type of functional ovarian cyst that forms after ovulation, during the normal menstrual cycle. Here’s how it happens:
- The Role of the Corpus Luteum
- After an egg is released from the ovary during ovulation, the follicle that held the egg doesn’t just disappear. Instead, it transforms into a structure called the corpus luteum (Latin for “yellow body”). The corpus luteum produces hormones like progesterone and estrogen, which help prepare the uterus for a possible pregnancy.
- How a Corpus Luteum Cyst Forms
- Sometimes, instead of breaking down and shrinking as it normally would if pregnancy doesn’t occur, the corpus luteum sticks around and fills with fluid. When this happens, it turns into a corpus luteum cyst. This is usually a harmless and temporary condition.
- Signs and Symptoms
- Most corpus luteum cysts are small, painless, and disappear on their own within a few weeks or months without causing any issues. However, if the cyst grows larger, it may cause symptoms such as:
- Pelvic pain: Usually mild and on one side of the lower abdomen.
- Fullness or heaviness in the abdomen.
- Menstrual changes: Irregular bleeding or spotting.
- When Things Get Complicated
- In rare cases, a corpus luteum cyst can cause problems: Cyst Rupture:
- If the cyst bursts, it can cause sudden, sharp pain and possibly internal bleeding. This might require medical attention.
- Ovarian Torsion:
- If the cyst is large, it can twist the ovary, cutting off its blood supply. This is a medical emergency and requires immediate treatment.
- Diagnosis and Treatment: Most corpus luteum cysts are discovered during routine ultrasounds or evaluations for pelvic pain. On ultrasound, they appear as fluid-filled sacs.
The Good News:
Both follicular cysts and corpus luteum cysts are like houseguests who know when it’s time to leave. They rarely stick around for more than a couple of months and don’t typically require treatment. Your body just takes care of business as usual.
When They Misbehave:
Although functional cysts are usually drama-free, they can sometimes cause:
- Pelvic Pain: Especially if they grow larger than usual.
- Cyst Rupture: This can cause sudden, sharp pain and might need medical attention.
- Ovarian Torsion: In rare cases, a larger cyst can cause the ovary to twist, cutting off its blood supply. This is a medical emergency.
So while functional cysts are natural and self-limiting, it’s always good to keep an eye on your symptoms and let your doctor know if you notice anything unusual.
B) Dermoid Cysts (a.k.a. “The Weird Ones”):
Dermoid cysts are the ultimate overachievers of the ovarian cyst world—and not in a good way! These fascinating (but slightly creepy) cysts are also known as mature cystic teratomas and can develop some very unexpected contents.
What Are Dermoid Cysts?
Unlike most ovarian cysts, which are just filled with fluid, dermoid cysts are made of cells called germ cells—the same type of cells that create eggs. Germ cells are pretty versatile and have the ability to form all kinds of tissue. In the case of dermoid cysts, these cells can go rogue, leading to the growth of hair, teeth, skin, fat, or even bone inside the cyst. Yep, you could have a tiny patch of hair or a tooth chilling in your ovary.
Dermoid cysts are typically benign (non-cancerous), so while they might sound like the stuff of nightmares, they’re not usually harmful.
Who Gets Dermoid Cysts?
More common in younger women: These cysts often show up during the reproductive years, typically in women under 30.
They can develop in one or both ovaries.
Signs and Symptoms
Most dermoid cysts are silent and go unnoticed until they’re discovered during a routine check-up or ultrasound. However, if they grow large enough, they can cause symptoms like:
Pelvic Pain: Especially on one side of the lower abdomen.
Feeling of Fullness: If the cyst presses on nearby organs.
Pain During Sex or Periods: Particularly if the cyst is sizable.
If a dermoid cyst twists the ovary (ovarian torsion) or bursts (ruptures), it can cause intense, sudden pain and might require immediate medical attention.
Diagnosis
Dermoid cysts are typically identified using an ultrasound, where they might appear as a mass with unusual echoes (because, let’s face it, teeth and hair inside a cyst look pretty weird). If further investigation is needed, doctors might use a CT scan or MRI to confirm.
Treatment
While dermoid cysts are harmless most of the time, they don’t go away on their own like functional cysts. Treatment depends on the cyst’s size and symptoms:
Watch and Wait:
If the cyst is small and not causing any problems, your doctor might suggest keeping an eye on it with periodic ultrasounds.
Surgical Removal:
If the cyst grows large, causes symptoms, or is at risk of complications, it may need to be removed.
This is usually done with laparoscopy (minimally invasive surgery), involving tiny incisions and a quick recovery.
Can Dermoid Cysts Be Dangerous?
Dermoid cysts are mostly harmless, but in rare cases, they can lead to complications like:
Ovarian Torsion: Larger cysts can twist the ovary, cutting off its blood supply—a medical emergency.
Rupture: If the cyst bursts, it can cause pain and irritation in the abdomen, as the contents spill into the belly.
Fun (and Creepy) Fact
Dermoid cysts aren’t just found in ovaries—they can pop up in other parts of the body, like the skin or spine. However, when they grow in the ovaries, they’re by far the most bizarre because of their ability to develop fully formed teeth, bones or other types of tissue.
The Bottom Line
Dermoid cysts might be nature’s version of a Frankenstein experiment, but they’re usually benign and manageable. If you’ve got one, don’t panic—your ovary might just be showing off its creativity. Still, it’s a good idea to keep an eye on it and talk to your doctor if you experience any symptoms.
Can Dermoid Cysts Be Cancerous?
Yes, but the chances are very low. When a dermoid cyst becomes cancerous, it is called a malignant transformation. This usually occurs in a specific type of cancer known as squamous cell carcinoma, which develops from the skin-like tissues inside the cyst.
How Rare Is It?
- Malignant transformation of dermoid cysts occurs in 1-2% of cases.
- This risk is slightly higher in women who are postmenopausal or over the age of 50.
For younger women, especially those of reproductive age, the risk of cancerous transformation in a dermoid cyst is extremely low.
Risk Factors for Cancerous Transformation
While the exact cause of malignant transformation isn’t fully understood, some factors may increase the risk:
- Age: Women over 50 are at a higher risk.
- Cyst Size: Larger cysts (over 10 cm) might have a slightly higher risk of malignancy.
What to Watch For
A dermoid cyst that is growing rapidly, causing significant symptoms, or showing unusual features on imaging tests (e.g., irregular borders or solid components) may raise concerns for malignancy. Your doctor might recommend closer monitoring or removal of the cyst.
Diagnosis and Treatment
- Diagnosis: Suspicious cysts can be further evaluated with imaging tests (like CT scans or MRIs) and sometimes blood tests (e.g., CA-125, a marker associated with ovarian cancer).
- Treatment: If there’s any concern about cancer, the cyst is usually removed surgically, and the tissue is analyzed to confirm whether it’s benign or malignant.
The Bottom Line
Dermoid cysts are almost always benign, with only a 1-2% chance of becoming cancerous. Routine monitoring and timely removal of symptomatic or suspicious cysts can help reduce risks and ensure your health. If you have concerns about a dermoid cyst, it’s always best to discuss them with your doctor.
C) Endometriomas (a.k.a. “Chocolate Cysts”):
Endometriomas are a specific type of ovarian cyst that sound sweet by name but are anything but fun. Nicknamed “chocolate cysts” for their appearance, they are filled with thick, old, brown blood—kind of like melted chocolate (but definitely not the tasty kind).
What Are Endometriomas?
Endometriomas are cysts that develop as part of endometriosis, a condition where the tissue that normally lines the inside of the uterus (endometrial tissue) starts growing outside of it. In the case of endometriomas, this rogue tissue finds its way to the ovaries.
Every month during your menstrual cycle, this misplaced tissue responds to hormonal signals just like the tissue inside your uterus:
It builds up.
It breaks down.
It bleeds.
But unlike regular menstrual blood, which exits the body, the blood from this tissue has nowhere to go. Over time, it gets trapped and forms a cyst filled with old, thickened blood—creating an endometrioma.
Signs and Symptoms
Endometriomas can vary in size and impact. While some are small and cause no symptoms, others can lead to significant discomfort. Symptoms include:
Chronic Pelvic Pain: A dull ache or sharp pain, especially before and during your period.
Pain During Sex: Known as dyspareunia, it’s a common symptom of endometriosis and endometriomas.
Heavy or Irregular Periods: Endometriosis can make periods unpredictable and excessively heavy.
Infertility: Endometriomas can affect ovarian function, making it harder to conceive.
Bloating or Fullness: Especially if the cyst is large.
How Are Endometriomas Diagnosed?
Endometriomas are typically diagnosed through:
Ultrasound: They appear as cysts with a “ground glass” or cloudy appearance.
MRI: In complex cases, an MRI can give more detailed images.
Laparoscopy: This is a surgical procedure where a camera is inserted into the abdomen to confirm endometriosis and/or endometriomas.
Why Are Endometriomas Called “Chocolate Cysts”?
The term comes from their appearance. When these cysts are drained during surgery, the contents resemble dark, chocolate-like fluid due to the old, oxidized blood inside them.
Are They Dangerous?
Endometriomas themselves are usually benign (non-cancerous), but they can still cause issues:
Chronic Pain: The inflammation caused by endometriosis can lead to significant discomfort.
Ovarian Damage: Large or persistent endometriomas can damage healthy ovarian tissue, reducing fertility.
Increased Cancer Risk: Although rare, women with long-standing or large endometriomas have a slightly higher risk of developing ovarian cancer, particularly a type called clear cell carcinoma. Regular monitoring is essential.
Treatment Options
The treatment of endometriomas depends on factors like size, symptoms, and whether you’re trying to conceive:
Watchful Waiting: If the cyst is small and not causing symptoms, your doctor may suggest monitoring it with regular ultrasounds.
Hormonal Therapy: Birth control pills, IUDs, or medications that suppress ovulation can help manage symptoms and slow cyst growth.
Surgical Removal: If the cyst is large, causing pain, or affecting fertility, a laparoscopic cystectomy (removal of the cyst using minimally invasive surgery) may be recommended to remove the endometrioma.
Surgery can relieve pain and improve fertility, but there’s a risk of damaging ovarian tissue. Surgery also inherently carries risks with it – including risk of bleeding, infection, damage to surrounding organs, post operative complications.
Fertility Treatments: If infertility is a concern, your doctor may recommend options like IVF (in vitro fertilization) to bypass the challenges posed by endometriomas.
Living with Endometriomas
Dealing with endometriomas often means managing endometriosis as a whole. While there’s no permanent cure for endometriosis, treatments can help control symptoms and improve quality of life. Regular follow-ups with a healthcare provider are essential to keep an eye on cyst growth and manage any complications.
The Bottom Line
Endometriomas may not be the kind of “chocolate” anyone wants, but understanding their connection to endometriosis is key. If you experience persistent pelvic pain, painful periods, or other symptoms, it’s important to seek medical advice. With the right care, endometriosis and its cystic companions can be managed effectively!
D) Cystadenomas: The Divas of Ovarian Cysts
Cystadenomas are a type of ovarian cyst that develop from the cells on the outer surface of the ovary. These cysts can grow quite large—sometimes bigger than a watermelon! Unlike functional cysts, which are part of the normal menstrual cycle, cystadenomas are abnormal growths. They are usually benign (non-cancerous), but their size and potential complications can still make them quite the troublemakers.
Types of Cystadenomas
Cystadenomas come in a few main varieties, based on what they’re filled with and how they behave. The two most common types are serous cystadenomas and mucinous cystadenomas, but there are rarer subtypes as well.
1. Serous Cystadenomas
What’s Inside?: These cysts are filled with a watery, clear fluid (think of them as “water balloons”).
Appearance: They are thin-walled and can grow up to 5-10 cm in size, although some can get larger.
Behavior: Serous cystadenomas are usually benign, but in rare cases, they can become malignant (cancerous). When cancer develops, it’s referred to as serous cystadenocarcinoma.
Symptoms: Often asymptomatic, but large ones can cause pelvic pain, bloating, or pressure on nearby organs.
Treatment: Small, asymptomatic cystadenomas may just be monitored.
Large or symptomatic cysts often require surgical removal.
2. Mucinous Cystadenomas
What’s Inside?: These cysts contain a thick, jelly-like fluid (think of them as “jello balloons”).
Appearance: They can grow to massive sizes—sometimes weighing over 100 pounds!
Behavior: Like serous cystadenomas, they are usually benign but can occasionally turn malignant (mucinous cystadenocarcinoma).
Mucinous cystadenomas are more likely to be multilocular, meaning they have multiple chambers or compartments.
Symptoms: Symptoms are similar to serous cystadenomas and include pelvic pain, abdominal swelling, and pressure on organs like the bladder or bowel.
Treatment: Surgical removal is often necessary due to their potential to grow very large and cause complications like ovarian torsion.
3. Other Types of Cystadenomas
Borderline Tumors: Some cystadenomas fall into a gray zone called borderline ovarian tumors, meaning they’re not clearly benign or malignant. These require careful monitoring and, often, surgical treatment.
Brenner Tumors: Rare and typically small, these are another type of surface epithelial tumor that sometimes coexists with cystadenomas.
They are usually benign and found incidentally during imaging or surgery.
How Are Cystadenomas Diagnosed?
Pelvic Ultrasound: The first step to identify a cyst and assess its size, contents, and structure.
CT or MRI Scans: May be used for a more detailed view, especially for larger cysts.
Blood Tests: CA-125: A tumor marker that helps assess whether the cyst might be cancerous. It’s not definitive but can guide further investigation.
Symptoms of Cystadenomas
Cystadenomas can be sneaky and silent, especially when small. But as they grow, they may cause:
Abdominal Swelling: Large cysts can make your belly look distended.
Pelvic Pain: A dull ache or sharp pain, especially on one side.
Bloating or a feeling of fullness.
Pressure Symptoms: Larger cysts can press on the bladder (causing frequent urination) or bowel (causing constipation).
Treatment for Cystadenomas
Treatment depends on the cyst’s size, symptoms, and whether it’s suspected to be benign or malignant:
Watchful Waiting: If the cyst is small, asymptomatic, and clearly benign, your doctor may suggest regular monitoring with ultrasounds.
Surgery: Cystectomy: Removal of just the cyst, preserving the ovary.
Oophorectomy: Removal of the entire ovary, often recommended for larger or more complex cysts, or if malignancy is suspected.
Surgery can be done laparoscopically (minimally invasive) for smaller cysts or through a larger incision (laparotomy) for very large or suspicious cysts.
Are Cystadenomas Dangerous?
Benign Nature: Most cystadenomas are harmless and non-cancerous.
Size Matters: Their potential to grow very large can cause complications like:
Ovarian Torsion: Twisting of the ovary, cutting off its blood supply.
Rupture: Although rare, a ruptured cystadenoma can cause pain and internal bleeding.
Malignancy: While uncommon, serous and mucinous cystadenomas can sometimes become cancerous, so monitoring and timely treatment are essential.
The Bottom Line
Cystadenomas are like the overachievers of the ovarian cyst world—big, dramatic, and occasionally demanding attention. Most are benign and easily managed, but their size and potential for complications mean they shouldn’t be ignored. If you suspect or have been diagnosed with a cystadenoma, regular check-ups with your doctor can ensure it’s handled safely and effectively.
E) Polycystic Ovaries: https://montanaobgyn.com/understanding-pcos-a-comprehensive-guide/
- Not just one cyst but a whole bunch. This happens in a condition called Polycystic Ovary Syndrome (PCOS) and can mess with your hormones. ( I have a post on this – https://montanaobgyn.com/understanding-pcos-a-comprehensive-guide/ )
F) Ovarian Cancer: When Ovarian Cysts Take a Serious Turn
Ovarian cancer is a rare but serious condition that can sometimes arise from ovarian cysts or other abnormalities in the ovaries. It’s often called the “silent killer” because early symptoms are vague and easy to miss. Let’s break it down:
Types of Ovarian Cancer
There are three main types of ovarian cancer, categorized by the type of cells involved:
- Epithelial Tumors (90% of cases):
- These arise from the outer lining of the ovary.
- Includes serous carcinoma, mucinous carcinoma, endometrioid carcinoma, and clear cell carcinoma.
- Germ Cell Tumors (5% of cases):
- These originate from the egg-producing cells.
- More common in younger women and often treatable.
- Stromal Tumors (5% of cases):
- These come from the supportive tissue of the ovaries.
- Includes granulosa cell tumors, which often produce hormones.
How Common Is Ovarian Cancer?
- Ovarian cancer accounts for about 1.2% of all cancers in women.
- It’s the 5th leading cause of cancer death in women, largely due to late diagnosis.
- The lifetime risk of developing ovarian cancer is about 1 in 78, and the risk of dying from it is 1 in 108.
Diagnosis
Detecting ovarian cancer early is challenging. Here’s how it’s typically diagnosed:
- Imaging Tests:
- Ultrasound: Helps identify cysts or tumors and their characteristics.
- CT or MRI: Provides a detailed look at the ovaries and surrounding structures.
- Tumor Markers:
- CA-125: A blood test that measures levels of a protein often elevated in ovarian cancer. However, it’s not specific and can be elevated in benign conditions.
- Other markers include HE4, AFP, hCG, and LDH, depending on the tumor type.
- Biopsy:
- A definitive diagnosis is made through tissue analysis, often during surgery.
Treatment Options
Treatment depends on the cancer type and stage but often involves:
- Surgery:
- Removal of one or both ovaries, fallopian tubes, the uterus, and sometimes nearby lymph nodes.
- Chemotherapy:
- Often used after surgery to target remaining cancer cells.
- Drugs like carboplatin and paclitaxel are common.
- Targeted Therapy:
- Newer treatments like PARP inhibitors and anti-angiogenic drugs focus on specific cancer mechanisms.
- Radiation Therapy (Rare):
- Occasionally used for localized tumors but not common for ovarian cancer.
The Bottom Line
While ovarian cancer is rare, it’s important to monitor ovarian cysts and other abnormalities closely, especially if there are risk factors like a family history of cancer or genetic mutations (e.g., BRCA1/2). Early detection and regular check-ups can make a significant difference in outcomes.
RECAP:
When to Be Concerned
Most ovarian cysts are silent ninjas—you don’t even know they’re there. But sometimes they throw a party, and you’ll feel it. Symptoms might include:
- Pain: A dull ache or sharp jabs in your lower belly, especially on one side.
- Bloating: Your pants might feel tighter (ugh).
- Period Problems: Late, early, or just plain weird periods.
- Peeing or Pooping Issues: If a cyst presses on your bladder or bowel, it can make things… complicated.
- Pain During Sex: Not fun, and definitely a reason to check with your doc.
If a cyst bursts (ouch!) or twists (double ouch!), it can cause sudden, intense pain and might send you running to the ER.
When to Be Concerned
Most ovarian cysts are harmless and disappear on their own, but here’s when you should hit the brakes and call a doctor:
- Severe Pain: Especially if it comes out of nowhere.
- Fever or Vomiting: Could mean an infection or serious complication.
- Unexplained Weight Loss: Or feeling full really quickly—these can be signs of something more serious.
- Changes in Periods: Like heavy bleeding or spotting when you’re not supposed to.
- Family History of Cancer: If ovarian cancer runs in your family, keep an eye on those ovaries.
How Are Cysts Treated?
The treatment depends on the cyst and how much of a diva it’s being:
- Watch and Wait:
- Most cysts go away on their own. Your doctor might suggest waiting a few months and then doing another ultrasound.
- Medication:
- Birth control pills can help prevent new cysts from forming (birth control pills suppress ovulation).
- Surgery:
- If the cyst is large, painful, or suspicious, it might need to be removed. Don’t worry—most surgeries are minimally invasive (tiny cuts, quick recovery).
- Cancer Treatment (Rare):
- If there’s a chance the cyst is cancerous, your doctor will act fast to get you the care you need.
Interesting Facts About Ovarian Cysts
- Common as Coffee: Most women will have at least one cyst in their lifetime. It’s like a rite of passage.
- Not All Bad: Functional cysts are part of your body doing its job. They’re like a temporary coworker who doesn’t overstay their welcome.
- Not Always Preventable: But regular check-ups can catch them early.
The Bottom Line
Ovarian cysts are usually no biggie, but they can sometimes cause trouble. Know the signs, listen to your body, and don’t hesitate to see your doctor if something feels off.
Your ovaries are amazing little factories—just keep an eye on the extra “products” they might make!
