Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects millions of people worldwide. Despite its prevalence, it’s often misunderstood, underdiagnosed, and surrounded by myths. If you’re looking to unravel the complexities of PCOS, this comprehensive guide will provide you with the essential information about its causes, symptoms, diagnosis, and management.
What Is PCOS?
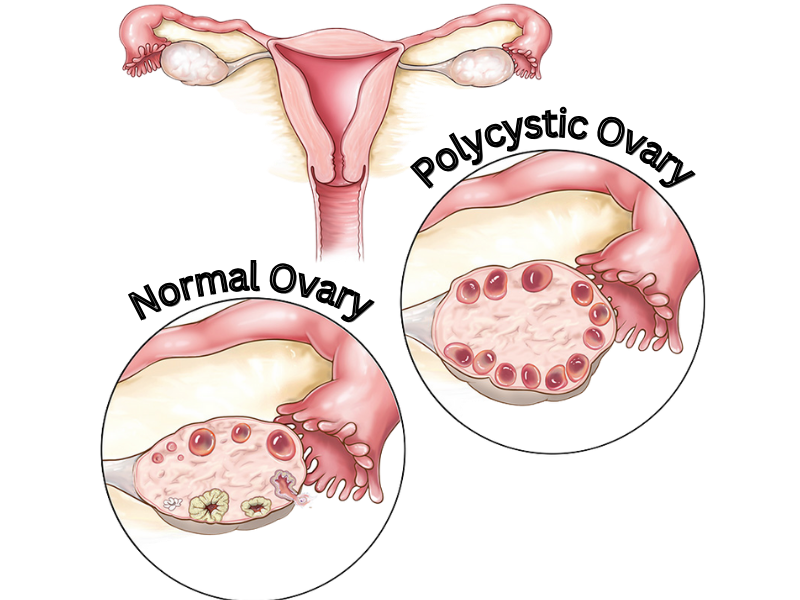
PCOS is a hormonal imbalance that affects how the ovaries function. The “polycystic” part of the name refers to multiple small, fluid-filled sacs (follicles) that may appear on the ovaries. These follicles are immature eggs that fail to develop or release during ovulation, often causing irregular menstrual cycles.
It’s important to note that not everyone with PCOS has these cysts, and the presence of ovarian cysts alone does not confirm the diagnosis.
What Causes PCOS?
The exact cause of PCOS isn’t fully understood, but it’s thought to involve a combination of genetic and environmental factors. Key contributors include:
- Hormonal Imbalance:
- Excess Androgens: Higher levels of male hormones (like testosterone) can interfere with ovulation and cause symptoms like acne and excess body hair.
- Insulin Resistance: Many people with PCOS have insulin resistance, which means their bodies produce more insulin to compensate. High insulin levels can increase androgen production.
- Genetics:
PCOS often runs in families, suggesting a genetic link. - Inflammation:
Chronic low-grade inflammation is common in PCOS and may contribute to increased androgen levels.
Common Symptoms of PCOS
PCOS symptoms can vary widely but often include:
- Irregular Periods:
- Infrequent, prolonged, or absent periods due to irregular ovulation.
- Excess Androgens:
- Symptoms like acne, excess facial/body hair (hirsutism), and male-pattern hair loss.
- Weight Gain:
- Many people with PCOS struggle with weight gain, especially around the abdomen.
- Polycystic Ovaries:
- Enlarged ovaries with small follicles visible on ultrasound.
- Fertility Issues:
- Difficulty getting pregnant due to irregular ovulation or anovulation (not ovulating).
- Skin Changes:
- Darkened skin patches (acanthosis nigricans), often found on the neck, armpits, or groin.
- Mood Changes:
- Anxiety and depression are more common in people with PCOS.
How Is PCOS Diagnosed?
There’s no single test for PCOS, so diagnosis involves ruling out other conditions and meeting specific criteria. Doctors typically use the Rotterdam Criteria, which require at least two of the following:
- Irregular or absent ovulation (oligo/anovulation).
- Elevated androgen levels (hyperandrogenism), either through blood tests or visible symptoms like hirsutism.
- Polycystic ovaries visible on ultrasound.
Other tests may include:
- Blood Tests: To measure hormone levels, glucose tolerance, and cholesterol.
- Pelvic Ultrasound: To look for ovarian cysts.
What Can PCOS Cause?
If untreated or unmanaged, PCOS can lead to various complications (or better said, these conditions are often associated with PCOS), including:
- Infertility: Irregular ovulation makes conception challenging.
- Type 2 Diabetes: Due to insulin resistance.
- Metabolic Syndrome: Increases the risk of heart disease and stroke.
- Sleep Apnea: Especially in those with obesity.
- Endometrial Cancer: Long gaps between periods can lead to an overgrowth of the uterine lining.
- Mental Health Issues: Higher rates of anxiety and depression.
Managing and Treating PCOS
There’s no cure for PCOS, but it can be effectively managed with a combination of lifestyle changes, medications, and other therapies.
Lifestyle Changes
- Diet:
- Focus on whole, unprocessed foods.
- Incorporate complex carbohydrates, lean proteins, and healthy fats.
- Reduce added sugars and refined carbs.
- Exercise:
- Regular physical activity helps manage weight and improves insulin sensitivity.
- Aim for a mix of aerobic exercises and strength training.
- Weight Management:
- Losing just 5-10% of body weight can significantly improve symptoms.
Lifestyle Changes to Help Manage PCOS
While there’s no direct cure for PCOS, this chronic condition can significantly improve with targeted lifestyle changes. These changes can help manage symptoms, improve hormonal balance, and reduce the risk of long-term complications like diabetes and heart disease.
Nutrition and Diet
A healthy, balanced diet is crucial for managing PCOS, especially as insulin resistance is often a factor.
- Focus on Low-Glycemic Index (GI) Foods:
- Foods like whole grains, legumes, fruits, vegetables, and nuts help stabilize blood sugar levels.
- Avoid refined carbs like white bread and sugary snacks that can spike insulin.
- Incorporate Lean Proteins and Healthy Fats:
- Include fish, chicken, eggs, and plant-based proteins.
- Add healthy fats like avocados, olive oil, and nuts to promote satiety.
- Reduce Sugar and Processed Foods:
- Minimize added sugars and highly processed snacks that exacerbate insulin resistance.
- Anti-Inflammatory Foods:
- Include foods like berries, leafy greens, fatty fish (like salmon), and turmeric to combat inflammation common in PCOS.
Medications
- Hormonal Birth Control:
- Regulates periods and reduces androgen symptoms like acne and hirsutism.
- Metformin:
- Improves insulin sensitivity and helps regulate ovulation.
- Fertility Treatments:
- Clomiphene or Letrozole to stimulate ovulation.
- IVF for more advanced fertility support.
- Anti-Androgen Medications:
- Spironolactone can reduce excess hair and acne.
- Other Options:
- Eflornithine for facial hair.
- Topical treatments for acne.
- Laser treatment for hair removal
Natural and Alternative Therapies
- Supplements:
- Inositol, omega-3 fatty acids, and vitamin D may help with symptoms.
- Acupuncture:
- Some find it beneficial for regulating cycles and managing stress.
Long term Effects of PCOS:
Polycystic Ovary Syndrome (PCOS) is a chronic condition that, if unmanaged, can lead to several long-term health effects. While the symptoms of PCOS, like irregular periods and acne, may be the most noticeable initially, the condition can also increase the risk of serious health issues over time.
1. Metabolic Complications
- Insulin Resistance, Type 2 Diabetes, Gestational diabetes: Many people with PCOS have insulin resistance, which can progress to type 2 diabetes if left unmanaged. There is also an increased risk for gestational diabetes in pregnancy (https://montanaobgyn.com/understanding-gestational-diabetes/).
- Metabolic Syndrome: A cluster of conditions, including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, that raises the risk of heart disease and stroke.
2. Cardiovascular Risks
- High Blood Pressure: A common complication of insulin resistance and weight gain.
- High Cholesterol and Triglycerides: PCOS can lead to an unfavorable lipid profile, increasing the risk of heart disease.
- Heart Disease: The combination of metabolic syndrome, insulin resistance, and obesity elevates the risk of cardiovascular diseases.
3. Reproductive Issues
- Infertility: Irregular ovulation or lack of ovulation makes conception difficult.
- Endometrial Hyperplasia and Cancer: Prolonged irregular or absent periods can lead to a thickened uterine lining, increasing the risk of endometrial cancer. Regular periods (natural or medically induced) are essential to mitigate this risk.
4. Mental Health Challenges
- Depression and Anxiety: Hormonal imbalances, difficulty managing symptoms, and societal pressures can contribute to higher rates of depression and anxiety in people with PCOS.
- Body Image Issues: Symptoms like weight gain, acne, and hair loss can negatively impact self-esteem.
5. Sleep Disorders
- Obstructive Sleep Apnea (OSA): More common in people with PCOS, especially those with obesity, sleep apnea disrupts breathing during sleep and increases cardiovascular risks.
6. Pregnancy Complications
- Gestational Diabetes: A higher risk due to underlying insulin resistance.
- Preeclampsia: PCOS increases the risk of high blood pressure and complications during pregnancy.
- Miscarriage: The condition has been associated with a higher risk of early pregnancy loss.
7. Chronic Inflammation
PCOS is associated with low-grade chronic inflammation, which can exacerbate insulin resistance, cardiovascular disease, and other health conditions.
8. Weight Management Challenges
- Obesity: Many people with PCOS struggle with weight gain due to hormonal imbalances and insulin resistance. This, in turn, exacerbates other PCOS-related risks.
9. Hair and Skin Conditions
- Hair Thinning: Androgenic alopecia can lead to hair loss over time.
- Hirsutism: Excess hair growth on the face and body can persist.
- Acne: Hormonal imbalances may result in persistent or severe acne.
Proactive Management Can Mitigate Risks
The good news is that many of these long-term effects can be prevented or managed with early intervention, lifestyle changes, and medical treatments.
- Maintain a Healthy Lifestyle: A balanced diet and regular exercise improve insulin sensitivity, support weight management, and reduce cardiovascular risks.
- Regular Medical Checkups: Monitor blood sugar levels, cholesterol, and blood pressure to catch complications early.
- Hormonal Treatments: Birth control or other medications can regulate menstrual cycles and reduce the risk of endometrial cancer.
- Mental Health Support: Therapy or counseling can help address anxiety, depression, and body image concerns.
Living with PCOS: Tips for Thriving
- Educate Yourself: Knowledge is power! The more you understand PCOS, the better you can advocate for yourself.
- Track Your Symptoms: Use apps or journals to monitor periods, mood, and other symptoms.
- Seek Support: Join PCOS communities or talk to a counselor for emotional support.
- Work with a Specialist: An endocrinologist or OB/GYN can tailor treatment to your needs.
Witty Facts About PCOS
- PCOS doesn’t mean you have to have cysts. It’s more about hormones than ovaries!
- PCOS affects 1 in 10 people with ovaries, but many don’t know they have it.
- Insulin resistance plays such a big role in PCOS that it’s often compared to “diabetes of the ovaries.”
Final Thoughts
PCOS can be challenging, but with the right support, treatment, and lifestyle adjustments, it’s entirely manageable. Whether you’re trying to conceive, balance hormones, or just feel better in your skin, remember—you’re not alone, and help is available. Reach out to your healthcare provider to start crafting a plan that works for you!

2 Responses